Don’t underestimate your risk of shingles
90% of people over 50 carry the virus that causes shingles.2†
If you’ve had chickenpox, the virus could reactivate at any time. Your risk increases sharply after 50, as your
immune system is less able to keep the virus dormant.1,3
†Not everyone at risk will develop shingles.1
Some underlying medical conditions can increase your risk.1
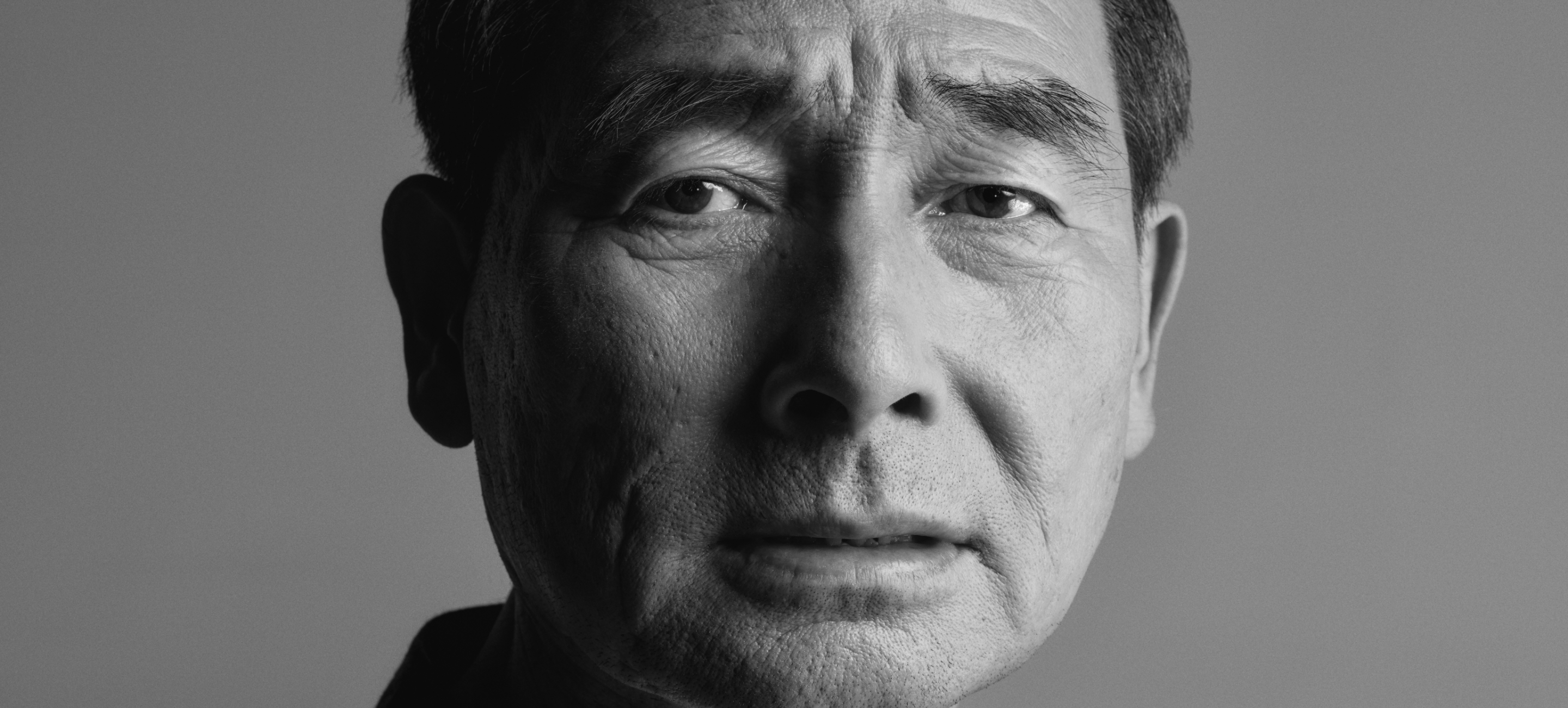
Hear more from Bil, a patient who's
experienced shingles suffering
Bil is a patient advocate and was diagnosed with shingles in 2024. This is his experience; others' experiences with shingles may be different.*
*Not everyone at risk will develop shingles.1
Shingles pain can last weeks or even months.1
Shingles symptoms may vary among patients.1
All images across the webpage are patient portrayals.
Any information provided on this website should be discussed with a healthcare professional and does not replace a healthcare professional's advice.
For more information or for medical advice, please consult a healthcare professional.
References
- Harpaz R, Ortega-Sanchez IR, Seward JF. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57(RR-5): 1–30.
- Bollaerts K, Riera-Montes M, Heininger U, et al. A systematic review of varicella seroprevalence in European countries before universal childhood immunization: deriving incidence from seroprevalence data. Epidemiol Infect. 2017;145:2666–2677.
- Hales CM, Harpaz R, Ortega-Sanchez I, Bialek SR. Update on recommendations for use of herpes zoster vaccine. MMWR Morb Mortal Wkly Rep. 2014;63(33):729–731.
- Huang CT, Lee CY, Sung HY, et al. Association between diabetes mellitus and the risk of herpes zoster: A systematic review and meta-analysis. J Clin Endocrinol Metab. 2022;107:586–597.
- Poirrier JE, Meyers JL, Nagar SP, et al. Herpes zoster incidence and burden in adults with type 2 diabetes in the USA: retrospective database analysis. Diabetes Care. 2022;45:2585–2593.
- Muñoz-Quiles C, Lopez-Lacort M, Ampudia-Blasco FJ, et al. Risk and impact of herpes zoster on patients with diabetes: A population-based study, 2009–2014. Hum Vaccin Immunother. 2017;13:2606–2611.
- Forbes HJ, Bhaskaran K, Thomas S L, et al. Quantification of risk factors for postherpetic neuralgia in herpes zoster patients: A cohort study. Neurology. 2016;87:94–102.
- Marra F, Parhar K, Huang B, Vadiamudi N. Risk factors for herpes zoster infection: A meta-analysis. Open Forum Infect Dis. 2020;7:ofaa005.
- Safonova E, Yawn B, Welte T, Wang C. Risk factors for herpes zoster: should people with asthma or COPD be vaccinated? Respir Res. 2023;24:35
- Yang YW, Chen YH, Wang KH et al. Risk of herpes zoster among patients with chronic obstructive pulmonary disease: a population-based study. CMAJ 2011;183:E275–280.
- Bloechliger M, Reinau D, Spoendlin J et al. Adverse events profile of oral corticosteroids among asthma patients in the UK: cohort study with a nested case-control analysis. Respir Res. 2018;19:75.
- Erskine N, Tran H, Levin L, et al. A systematic review and meta-analysis on herpes zoster and the risk of cardiac and cerebrovascular events. PloS One. 2017;12:e0181565.
- Ishigami J, Matsushita K. Clinical epidemiology of infectious disease among patients with chronic kidney disease. Clin Exp Nephrol. 2019;23:437–447.
- Lin SY, Liu JH, Yeh CH, et al. Association between herpes zoster and end stage renal disease entrance in chronic kidney disease patients: a population-based cohort study. Eur J Clin Microbiol Infect Dis. 2014;33:1809–1815.
- Habel LA, Ray GT, Silverberg MJ. et al. The epidemiology of herpes zoster in patients with newly diagnosed cancer. Cancer Epidemiol Biomarkers Prev. 2013;22:82–90.
- Winthrop K, Curtis J, Yamaoka K, et al. Clinical management of herpes zoster in patients with rheumatoid arthritis or psoriatic arthritis receiving tofacitinib treatment. Rheumatol Ther. 2022;9:243–263.